Sporotrichosis is known as Sporo. Sporotrichosis is a dimorphic fungi that exist in two distinct forms as a mould form in environment and as a yeast form in animals tissue. It is in the Moniliaceae family of Deuteromycete class of fungi. It is environmental acquired disease. It also known as ‘rose-growers’ disease. It is often observed in gardeners. It may develop via a thorn prick to the finger. The source of sporotrichosis is sphagnum moss. Commonly, the infection located in arms and can develop elsewhere.
Host range for infection :
- human
- horses
- dogs
- pig
- cats
- cattle
- camels
- fowl
- rats
- mice
- hamster
- mules ( cross of male donkey & female horse)
Sequence of Infection:
1. Inoculation with Sporothrix Schenckii via pricking of a finger
2. A pustule develops and ulcerates
3. Infection invades a pustule the lymphatic system and ascends the arms
4. Result of a chain of cutaneous ulcers.
6 factors important factors that influence the emergence of zoonotic disease :
1.Transportation of humans, animals between geographic locations.
2. Increased contact between animals and human.
3. Changes in the environment and husbandry practice.
4. A growing population of immunocompromised humans.
5. Increased awareness of zoonotic origin of many diseases
6. the identification of organisms that were not previously known.
2 important mechanism ( its potential to infect the mammalian host is maximised.)
1. Has ability to change phases to ascomycete telemorph that survives on living/ decaying plant materials.
2. Convert to yeast phase (after entering skin via puncture, bite, scratch)
Transmission :
1. Subacute-chronic cutaneous and subcutaneous infection.
2. Skin exposure by stratch, puncture wound, abrasion.
3. Development of a papule that enlarges to nodule & usually ulcerates over a period of 1-2 weeks.
4. If not treated, infection may progress to lymphatic system and cause the lymphocutaneous form of sporotrichosis.
5. Extracutaneous form of sporotrichosis often seen in patients :
- alcoholism
- diabetes mellitus
- chronic obstructive pulmonary disease.
- human immunodeficiency virus infection.
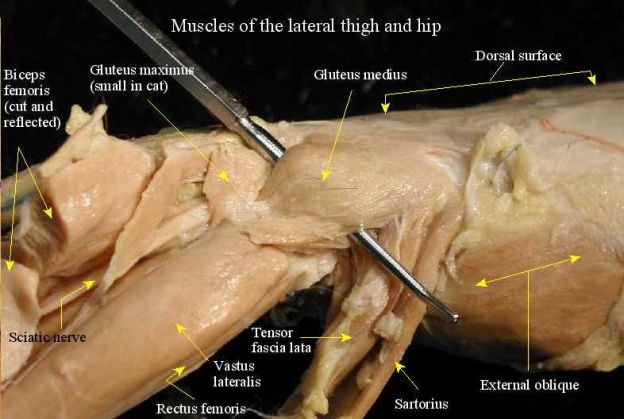
In cats, usually exposed via wound contamination or penetrating foreign bodies.
Clinical signs/syndromes in feline sporotrichosis :
- localised (common in cats. It is confined to area of inoculation & develops after incubation period of approximately 1 month. If it is not treated, it will be progress into lymphcutaneous form. latter, cutaneous nodules progress to draining ulcers that affect skin, subcutis, regional lymphatics, lymph node) or fixed cutaneous lesions. ( cutaneous lesions often observed in legs, face and nasal plenum)
- lymphocutaneous (common in cats).
- multifocal disseminated sporotrichosis. ( lung and liver are primary site of disseminated sporotrichosis).
Differential diagnosis of skin lesions in cats may include :
- bacteria pyoderma
- mycobacteriosis
- actinomycosis
- cryptococcosis
- sporotrochosis
- foreign body
- squamous cell membrane
- immune-mediated carcinoma
- immune-mediated disease
- systemic lupus erythematosis
- pemphigus vulguris
- allergy
- allergy to parasites
- drug eruption
Diagnosis
- Cytologic evaluation of sample ( aspiration of abscess/nodules, impression smear of ulcerated skin/ exudate, smear of swab specimen, skin scraping). Its characteristics : Oval, 3-5 mm in diameter, 5-9 mm in length, cigar-shaped, bu may appear as round budding yeast.
- Fungal culture on Sabouraud mycologic medium ( swabs, biopsy specimen lesion) and incubated in both 25 C and 27 C for 10-14 days.
- Serologic testing’
- Indirect fluorescent antibody testing
- Histologic examination of fixed biopsy specimens of lesions.
Treatment :
- Antimicrobial treatment
- Sodium Iodide ( but it is replaced with more effective and safer antifungal drugs : Imidazoles )
- Imidazoles
- Ketaconzote ( not complete elimination, its effects are anorexia, weight loss)
- Itraconazole ( orally : 5-10 mg/kg ( 2.5-4.5 mg/lb) every 12 hours)
Prevention and Control :
- Always wear gloves when handling cats with ulcerative lesions or open draining tracts.
- Wash hands and arms with antiseptic.